Connect With Us
Featured Articles

Problematic Flat Feet

Flat feet, or fallen arches, occur when the arch of the foot is lower than normal. Children are often born with flat feet, and in most cases, the condition naturally resolves by the age of seven to 10 as the foot develops. Flat feet are classified based on arch height and heel aversion angle and can be either flexible or rigid. In flexible flat feet, the arch appears when the foot is lifted but disappears when standing, while rigid flat feet have no arch even when off the ground. Flat feet can be caused by genetics, injury, or conditions like arthritis. Symptoms include foot pain, particularly in the heel or arch, and difficulty standing for long periods. Pain occurs due to abnormal pressure on muscles and ligaments. Treatment includes supportive footwear, orthotics, and targeted stretching. In severe cases, surgery may be considered to correct alignment and relieve discomfort. If you have painful flat feet, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from APEX Foot & Ankle Center. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Fort Myers, Cypress Cove, Shellpoint, Naples, and Carlisle, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is Flexible Flat Foot?
Flatfoot is classified as having the entire sole of the foot in contact or near contact to the ground while standing. The disorder is also known as fallen arches, because those affected have no arch in their feet. Flexible flatfoot and rigid flatfoot are the two types of flatfoot.
A person has flexible flatfoot if when sitting or standing on their toes, they have an arch that disappears when they stand with the entire foot on the ground. Flexible flatfoot may also be called “pediatric flatfoot” because the condition first appears in childhood. It is common among infants because the arch does not develop until the age of 5 or 6 years. Rigid flatfoot is not as common in children as it is with adults. This type of flatfoot is developed due to the weakening of tibialis posterior muscle tendon, a major supporting structure of the foot arch. Development of this deformity is progressive and shows early signs of pain and swelling that begins at the inside arch of the foot and moves to the outside of the foot below the ankle. More severe cases can possibly lead to arthritis of the foot and ankle joints.
Although most cases of flatfoot involve people born with the condition, some less common causes are obesity, diabetes, pregnancy, and osteoporosis. In some cases, flatfoot may come with no symptoms at all and does not require any type of treatment. With other cases though, symptoms may include pain in the shin, knee, hips and lower back. If a person with flatfeet experiences such symptoms, a health care provider may suggest using orthotic devices or arch supports, which may reduce the pain. Wearing supportive shoes can also prove more comfortable with flatfeet and staying away from shoes with little support such as sandals. Other methods to relieve pain also include stretching the Achilles tendon properly and using proper form when doing any physical activity. In addition, losing weight can reduce the stress on your feet and reduce the pain.
How Diabetes Affects the Feet

Diabetes can significantly impact foot health, primarily through a condition known as diabetic neuropathy. This occurs when high blood sugar levels damage the nerves in the feet, leading to symptoms like numbness, tingling, and pain. In severe cases, diabetic patients might experience a loss of sensation, making it difficult to detect injuries or infections. Additionally, poor circulation can slow down healing, which increases the risk of ulcers and infections. Proper management of blood sugar levels is key to preventing these complications. Regular foot inspections, wearing proper footwear, and daily foot care can help mitigate the effects. Treatment often involves managing diabetes effectively, controlling pain with medications, and in some cases, foot exercises. To ensure optimal foot health and address any concerns, it is suggested you schedule an appointment with a podiatrist for specialized care and preventive strategies tailored to your needs.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from APEX Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Fort Myers, Cypress Cove, Shellpoint, Naples, and Carlisle, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Conditions
According to the American Diabetes Association (ADA), diabetes is a condition that affects approximately 23.6 million Americans. Around 750,000 new cases are diagnosed each year, and the disease’s most common form, Type 2 diabetes, makes up for 90 to 95 percent of these cases. Type 2 diabetes is especially prevalent among older Americans, those who are obese, and those who lead sedentary lifestyles.
Complications of the disease may lead to several foot and ankle-related conditions. The loss of nerve sensation, or neuropathy, can cause diabetics to lose feeling at the bottom of the feet and therefore leave them unaware of pain, pressure, and heat. Decreased circulation is another complication of diabetes that can slow down the healing of wounds and injuries; this can lead to the development of foot ulcers.
To prevent foot ulcers from forming, diabetics should examine their feet every day for small cuts and wear shoes that curtail pressure. Constant monitoring for the risk factors associated with ulcer formation can allow for early detection and therefore lessen the possibility of ulcers or, even worse, amputation. The removal of calluses and ingrown toenails should be left to the podiatrist to avoid improper removal and possible infection.
Diabetic patients may also experience foot deformities due to complications in their feet, such as limited joint mobility, muscle atrophy, and decreased fat padding. These complications can increase pressure in certain areas of the foot, which in turn can cause certain deformities, such as hammertoe, to form. Another deformity, Charcot foot, develops due to the collapsing of microfractures in the bones of the feet. The resulting deformity is a foot that is flattened and wider in appearance.
To help minimize pressure and prevent the development of these diabetes-related foot and ankle conditions, your podiatrist may consider using orthotics or special shoes. Charcot foot may be treated using walkers, custom orthotic insoles, or non-weight-bearing or rigid weight-bearing casts or braces. In more serious cases, surgery may be considered to treat more developed deformities. Ulcers can be further cared for with the help of proper diet, medication to control glucose, intensive wound care, and infection treatment.
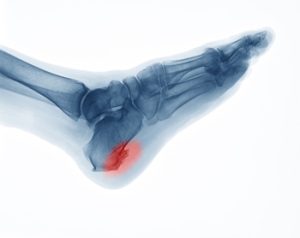
Types and Symptoms of Heel Spurs
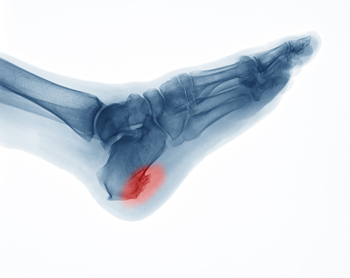
Heel spurs are bony protrusions that form on the heel bone, or calcaneus. The two primary types are plantar and dorsal heel spurs. Plantar heel spurs develop on the bottom of the heel, where the plantar fascia attaches to the bone, often causing pain in the arch or heel. Dorsal heel spurs form on the back of the heel and can lead to discomfort in the Achilles tendon area. Common symptoms include sharp or aching pain, particularly with movement or pressure. The primary causes of heel spurs are repetitive strain, improper footwear, or conditions such as plantar fasciitis. Overuse or excessive stress can trigger inflammation and heel spur formation. If you have heel pain, it is suggested that you schedule an appointment with a podiatrist who can provide a proper diagnosis and treatment.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from APEX Foot & Ankle Center. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Fort Myers, Cypress Cove, Shellpoint, Naples, and Carlisle, FL . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
Facts About Morton’s Neuroma

Morton’s neuroma is a painful condition affecting the nerves in the ball of the foot, typically between the third and fourth toes. This condition occurs when the tissue around the nerve thickens due to irritation or pressure, often from wearing tight or high-heeled shoes. Symptoms of Morton's neuroma include sharp pain, burning, or a sensation like stepping on a small stone. Numbness or tingling in the toes can also be experienced. Risk factors include wearing narrow footwear, having foot conditions like flat feet or bunions, or engaging in high-impact sports. A podiatrist can provide custom orthotics, lifestyle modifications, or non-invasive therapies to alleviate discomfort and prevent long-term damage. If left untreated, Morton’s neuroma can lead to chronic pain and permanent nerve damage, like numbness in the toes. If you have pain in the ball of the foot that may be from Morton’s neuroma, it is suggested that you make an appointment with a podiatrist for an exam, diagnosis, and treatment options.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of APEX Foot & Ankle Center. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Fort Myers, Cypress Cove, Shellpoint, Naples, and Carlisle, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Facts About Ingrown Toenail Surgery and Prognosis

Ingrown toenail surgery is a common procedure to treat toenails that have grown into the surrounding skin, causing pain and potential infection. The surgery typically involves removing part or all of the affected toenail and, in some cases, treating the nail bed with a chemical or surgical method to prevent regrowth. The procedure is usually performed under local anesthesia, ensuring minimal discomfort. Post-surgery, patients may experience some pain, swelling, and redness, but these symptoms generally improve within a few weeks. The prognosis for ingrown toenail surgery is generally positive, with most individuals experiencing significant relief from pain and discomfort. Proper foot care and following post-operative instructions are essential for a successful recovery and to prevent recurrence. If you have an ingrown toenail, it is suggested that you make an appointment with a podiatrist who can determine if surgery is right for you.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact one of our podiatrists of APEX Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our offices located in Fort Myers, Cypress Cove, Shellpoint, Naples, and Carlisle, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Featured Articles
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016